Overview
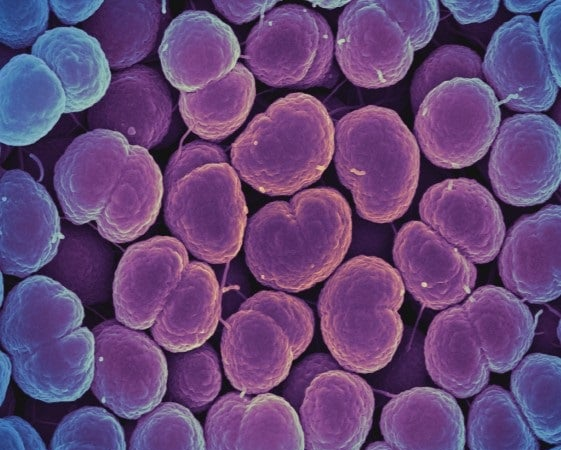
Gonorrhoea is a sexually transmitted infection (STI) that remains a major public health concern. WHO estimates that in 2020, there were 82.4 million [47.7 million-130.4 million] new cases infected among adolescents and adults aged 15–49 years worldwide, with a global incident rate of 19 (11–29) per 1000 women and 23 (10–43) per 1000 men. Most cases were in the WHO African Region and the Western Pacific Region.
Antimicrobial resistance (AMR) in Neisseria gonorrhoeae (N. gonorrhoeae) appeared soon after the antimicrobial medicines started to be used. This has continued to expand over the past 80 years, affecting medicines such as tetracyclines, macrolides (including azithromycin), sulphonamides and trimethoprim combinations and, more recently, quinolones. In many countries, ciprofloxacin resistance is exceedingly high, azithromycin resistance is increasing and resistance or decreased susceptibility to cefixime and ceftriaxone continue to emerge.
The extensively drug-resistant gonorrhoea with high-level resistance to the current recommended treatment for gonorrhoea (ceftriaxone and azithromycin) but also including resistance to penicillin, sulphonamides, tetracycline, fluoroquinolones and macrolides are called gonorrhoea superbugs or super gonorrhoea.
History
The first reported treatment failure with cefixime was in Japan. In the past decade, confirmed failure to cure gonorrhoea with ceftriaxone alone or combined with azithromycin or doxycyline was reported in Australia, France, Japan, Slovenia, Sweden and the United Kingdom of Great Britain and Northern Ireland. In 2016, the first global failure to cure pharyngeal gonorrhoea with dual therapy (ceftriaxone 500 mg plus azithromycin 1 gram) was confirmed in the United Kingdom. An international spreading ceftriaxone-resistant gonococcal strain has been reported in Denmark, France, Japan and United Kingdom. In 2018, the first global gonococcal strains with ceftriaxone resistance and high azithromycin resistance causing pharyngeal gonorrhoea was reported in the United Kingdom. There are increasing numbers of treatment failure cases being reported from United Kingdom, Austria and other countries.
All confirmed treatment failures except one recent case in the United Kingdom have been pharyngeal infections affecting the throat. The majority of infections in the pharynx are asymptomatic. Antimicrobial drugs don’t penetrate the tissue well in that area, and the pharynx is also home to naturally occurring related bacteria of the Neisseria species that can contribute to drug resistance. Most data on this issue come from higher income countries; however, the majority of cases of gonorrhoea are in less resourced countries and areas. This suggests that reports of treatment failures and drug resistance in wealthier areas are only the tip of the global health burden. Surveillance data on antibiotic resistance and treatment failures from poorer countries are exceedingly scarce and need to be improved. High rates of antimicrobial resistance to penicillins, tetracyclines and quinolones have been known for a longer time, and these medicines are currently not recommended for the treatment of gonorrhoea in most countries around the world.
Resistance to so many treatment options, including penicillins, sulphonamides, tetracyclines, quinolones and macrolides (including azithromycin), as well as so-called last line options like cephalosporins, make N. gonorrhoeae a multidrug resistant organism.
This resistance is caused by a number of factors, including unrestricted access to antimicrobials, inappropriate selection and overuse of antibiotics, and poor quality antibiotics. Further, genetic mutations within the organism have contributed to increased drug resistance in N. gonorrhoeae. Infections outside of the genital area – namely in the throat and rectum – particularly affect key populations such men who have sex with men. This may also play an important role in the development of resistant strains as N. gonorrhoeae interact and exchange genetic material with other organisms in these parts of the body.
Implications
Gonococcal infections have critical implications to reproductive, maternal and newborn health including:
The financial costs of these complications are very high for both individuals and health care systems. Antimicrobial resistance increases this burden by prolonging the infection in more people and increasing the number of people with long-term complications of gonococcal infections.
The emergence of different forms of resistance in N. gonorrhoeae is often followed by a rapid spread of the disease. This is not a problem only of the poor, and recent treatment failures have also been seen in higher income countries. Since it can be difficult to find complete information from areas with limited resources for surveillance, the antimicrobial resistance is expected to be much higher than what is currently seen due to silent spreading.
WHO response
Fighting multidrug-resistant N. gonorrhoeae requires 2 approaches: broad control of drug resistance and control of gonorrhoea. Both should be approached in the wider contexts of global control of antimicrobial resistance.
WHO is implementing the Global Action Plan to Control the Spread and Impact of Antimicrobial Resistance in N. gonorrhoeae to facilitate effective actions against the spread of multi-drug resistant N. gonorrhoeae. This Plan is part of the greater STI surveillance plan to help early detection of emerging resistant strains, combined with a public health response to prevent and treat gonococcal infections and reduce the impact of gonorrhoea on sexual and reproductive health.
The Global Health Sector Strategy on HIV, Hepatitis and STIs (2022–2030) has set targets to reduce the number of new cases of gonorrhoea among people 15–49 years old from 82.3 million per year in 2020 to 8.23 million per year in 2030, thus reducing the year incidence by 90% by 2030. Recognizing that this reduction may be difficult to achieve with available interventions, and given increasing antimicrobial resistance, the strategy has emphasized the need to develop effective gonococcal vaccines. No currently licensed gonococcal vaccines exist. However, interest in gonococcal vaccine development has been reinvigorated not only by the marked increases in gonococcal antimicrobial resistance, but also by mounting scientific evidence suggesting gonococcal vaccines are biologically feasible.
The key WHO actions are:
WHO will continue to work with Member States and partners to understand and reduce antimicrobial resistance through better control of antibiotic medications and actions to prevent the spread of gonorrhoea.
Related
Antimicrobial resistance
Sexually transmitted infections
Fact sheets







