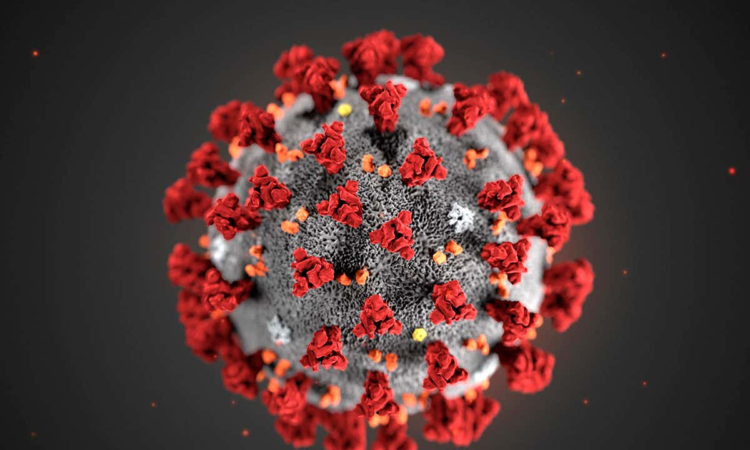
For the Harvard Chan community: Find the latest updates, guidance, useful information, and resources about Coronavirus Disease 2019 (COVID-19) here.
In the wake of an outbreak of coronavirus that began in China in 2019, Harvard T.H. Chan School of Public Health experts have been speaking to a variety of media outlets and writing articles about the pandemic. We’ll be updating this article on a regular basis. Here’s a selection of stories in which they offer comments and context:
February 20: COVID is still killing people every day. But its main victims have changed. (The Boston Globe)
Early in the pandemic, Black and Hispanic people were more likely than white people in Massachusetts to die from COVID, but that trend has now reversed. Yonatan Grad, Melvin J. and Geraldine L. Glimcher Associate Professor of Immunology and Infectious Diseases, commented on factors that may be driving the switch, such as better access to vaccines in communities of color in 2022 and improved access to care. Another factor may be a phenomenon called mortality displacement, in which an infectious disease outbreak temporarily increases death rates in a population and is followed by a period of lower mortality rates. William Hanage, associate professor of epidemiology, said that hybrid immunity—stronger immune protection among those infected after vaccination—may also be playing a role.
February 15: A new Harvard study says sticking to these 6 habits could cut your long COVID risk in half (Parade)
Siwen Wang, research fellow in the Department of Nutrition, discussed a study she led on how healthy habits—including maintaining a healthy body weight, not smoking, and exercising regularly—may reduce the risk of long COVID.
February 10: The COVID-19 public health emergency is ending. Now what for HR? (Human Resource Executive)
Jeffrey Levin-Scherz, assistant professor in the Department of Health Policy and Management, co-authored this piece about how employers’ strategies should currently address the pandemic, given evolving conditions.
February 9: She helped unlock the science of the COVID vaccine (The New York Times)
Kizzmekia Corbett, assistant professor of immunology and infectious diseases, was profiled for her work leading a team of scientists that contributed to the development of the COVID vaccine.
February 6: New research suggests simple steps to reduce long COVID symptoms (CBS News)
Adhering to five or six healthy lifestyle factors could significantly reduce the risk of long COVID, according to a new study from Harvard Chan School. Said co-author Andrea Roberts, senior research scientist in the Department of Environmental Health, “What if Americans had five or six of these healthy lifestyles instead of whatever they do have now? And we calculated that about 36% of long COVID cases could have been avoided.”
February 6: Healthy lifestyle may mean lower risk of long COVID, study says (CNN)
Siwen Wang, research fellow in the Department of Nutrition, quoted.
February 3: This winter’s U.S. COVID surge is fading fast, likely thanks to a ‘wall’ of immunity (NPR)
Immunity to COVID-19, both from vaccines and from prior infections, is likely the reason why this winter’s disease surge was much less severe than surges from past winters, according to experts. But they also warn that COVID still remains a threat. “It’s beyond question that society has moved into a stage where the pandemic is for most of us if not over then certainly quiet. And that’s a great thing. Long may it remain so,” said William Hanage, associate professor of epidemiology. “Is it the case that there is no preventable suffering? No. There is still preventable suffering and death.”
February 1: What the end of COVID emergencies means for older adults (AARP)
Anna Sinaiko, assistant professor of health economics and policy, was among experts discussing potential changes in health coverage, including costs for vaccines, tests, and treatments, when the COVID-19 public emergencies end in May.
February 1: The U.S. COVID-19 public health emergency ends in May. Here’s what will change (Time)
Ending the COVID-19 public health emergency will make it harder for some people—depending on their health insurance status—to access things like free vaccines, COVID-19 tests and treatments, and telehealth care. The change may also lead to higher hospital care costs for some COVID-19 patients. Health inequities could result, noted Jose Figueroa, assistant professor of health policy and management. “Will [the end of the public health emergency] change the trajectory of the pandemic?” he said. “It’s something we are going to have to watch.”
February 1: End of national emergencies brings new challenges to US COVID response (The National Desk)
Access to free testing will be one of the biggest changes when the COVID-19 public health emergency ends. Different people may have to pay different amounts for tests, depending on their insurance coverage. “It’s unclear what individual [health] plans will do but that’s a major, major change,” said Jose Figueroa, assistant professor of health policy and management. “There’s concerns that there’s going to be a lot less testing happening out in the community.” Access to free vaccines could also end for some, which could further quell vaccine uptake. “If when they’re free, not everyone’s taking them, can you imagine if you have to now pay for it?” he said. “It’s going to be less and that will contribute to potentially future outbreaks.”
February 1: What the End of the Covid Public Health Emergency Could Mean for You (New York Times)
Jose Figueroa, assistant professor of health policy and management, quoted.
January 30: FDA panel votes to make all COVID-19 shots bivalent (Everyday Health)
An advisory panel to the FDA recommended that all COVID-19 vaccines be the bivalent version going forward. The panel also discussed the possibility of establishing an annual COVID-19 booster shot—but held off. “I think it’s quite reasonable to think of another [update to the booster] for the fall [of 2023], but it’s hard to say that it’s going to be annual at this point,” said panel member Eric Rubin, adjunct professor of immunology and infectious diseases.
January 26: The COVID emergency might end after 3 long years – but the virus is still a threat (CBC)
Experts discussed how COVID will continue to threaten us for years to come. Although vaccinations, treatments, and prior immunity make COVID much less dangerous for most people, there are still those who remain vulnerable, including older people and other high-risk individuals. Bill Hanage, associate professor of epidemiology, noted that not much has been done to protect the most frail individuals living in nursing homes in North America. “I think that it’s kind of crazy that we [hadn’t] previously developed ways to robustly rapidly test people who work in nursing homes, to prevent them bringing in respiratory viruses,” he said.
January 19: Davos 2023: Chief executive of ‘world’s largest vaccine maker’ on the state of the pandemic (World Economic Forum)
Harvard Chan School Dean Michelle Williams was quoted.
January 19: Public health agencies are retooling as COVID-19 response winds down. A slim majority of adults trusts them to manage another pandemic (Morning Consult)
Vish Viswanath, Lee Kum Kee Professor of Health Communication, said that the CDC and other health institutions “have taken a real hit” in terms of trust during the pandemic. He cited politicization and communication mistakes among the reasons for the decline.
January 19: How scientists trained computers to forecast COVID-19 outbreaks weeks ahead (Los Angeles Times)
Mauricio Santillana, adjunct professor of epidemiology, and colleagues developed a machine learning system for predicting when and where COVID-19 outbreaks will occur. Said Santillana, “Our work is aimed at documenting what techniques and approaches might be useful not just for this [the COVID-19 pandemic], but the next pandemic.”
January 11: FDA vaccine advisers ‘disappointed’ and ‘angry’ that early data about new Covid-19 booster shot wasn’t presented for review last year (CNN)
Eric Rubin, adjunct professor of immunology and infectious diseases, was among members of an FDA advisory committee who expressed dismay that they weren’t told last year about data suggesting that Moderna’s then-new bivalent COVID booster may not be any more effective at preventing the disease than the original vaccines. The committee members said the information would have been important for them to have as they discussed whether or not the booster should be made available to the public. “It’s not a group of children,” Rubin said. “We understand how to interpret these results.”
January 10: Coronavirus FAQ: How do I avoid catching COVID while flying in 2023? (NPR)
With COVID surging in China and the highly contagious XBB variant circulating, experts are suggesting taking precautions when flying, such as wearing a high-quality mask. Leonard Marcus, founding co-director of the National Preparedness Leadership Initiative (NPLI) and co-director of NPLI’s Aviation Public Health Initiative, also recommended distancing during boarding and deplaning, wiping surfaces such as bathroom door handles and seat trays with alcohol wipes, and turning on air vents. “The ventilation pushes clean air from above to the floor,” he said. “The more of that the better.”
Learn more
See stories from:
November 2022
October 2022
September 2022
August 2022
July 2022
June 2022
May 2022
April 2022
March 2022
February 2022
January 2022
December 2021
November 2021
October 2021
September 2021
August 2021
July 2021
June 2021
May 2021
April 2021
March 2021
February 2021
January 2021
December 2020
November 2020
October 2020
September 2020
August 2020
July 2020
June 2020
May 2020
April 2020
March 2020
January and February 2020
Explore HSPH research by topic







